Minimum Stimulus Strategy in the Diagnosis of BPPV
Introduction
Benign Paroxysmal Positional Vertigo (BPPV) is the most common disease of the inner ear, presenting with a 10% cumulative lifetime incidence. According to the most widely accepted theory, it represents a “maculo-canalopathy” where dislodges otoconia fall from utricular macula into one or more semicircular canals (SCs), resulting in inappropriate activations of the involved ampullary receptors by linear accelerations such as gravity. The pathophysiological mechanism of BPPV is commonly ascribed either to free-floating particles within the SC (canalolithiasis) or to debris attached to the cupula of the affected SC (cupulolithiasis). In clinical practice, BPPV can be classified according to the affected SC and the involved arm, as follows:
- Posterior Semicircular Canal (PSC) BPPV: geotropic and apogeotropic variants
- Horizontal Semicircular Canal (HSC) BPPV: geotropic and apogeotropic variants
- Anterior Semicircular Canal (ASC) BPPV
The diagnosis of the affected canal should always be based on the step-by-step observation of the evoked nystagmus rather than on the provoking maneuver eliciting positional vertigo. According to the vestibulo-ocular reflex (VOR) pathophysiology, each cupular deflection, either exciting or inhibiting the corresponding ampullary afferents, generates the contraction of specific extraocular muscles couples leading to pathognomonic nystagmus. The diagnosis of the affected ear and the involved canal and arm is commonly based on positioning tests, also known as diagnostic maneuvers. Traditional diagnostic maneuvers move free-floating debris using both gravity and inertial/centrifugal forces which bend the cupula of the affected SC. Several maneuvers have been proposed to properly diagnose each BPPV variant moving the patient's head along the plane of the examined SC. However, a diagnostic maneuver recommended for assessing BPPV involving a specific SC could evoke a type of nystagmus suggesting the involvement of a different SC. Therefore, diagnosis should always be based on the evoked nystagmus rather than on the positioning test. The typical paroxysmal nystagmus is more easily evoked by examining the patient within the so-called “active period” (24 - 72 hours from the onset of symptoms). Nevertheless, in this “active period”, the diagnostic maneuvers might hardly be conducted in patients suffering from intense autonomic and anxiety-related symptoms. These last conditions might prevent from detecting the affected side and the involved canal/arm, especially in those cases where repeated positionings are usually needed. The Minimum Stimulus Strategy (MSS) represents a nystagmus-based approach aimed to reduce the number of diagnostic and therapeutic maneuvers required for the BPPV management and patient's discomfort.
AudiologyOnline: Which are the pathophysiological principles and the steps of the Minimum Stimulus Strategy in the diagnosis of BPPV?
Andrea Castellucci: MSS represents a diagnostic and therapeutic approach to BPPV that is conducted with continue monitoring of the evoked nystagmus by video-Frenzel goggles according to the head position changes. A key point of MSS is the Upright BPPV Protocol (UBP), consisting in diagnostic tests performed with the patient in the sitting position and slowly bending his head around the spatial axes to move canaliths by gravity along the involved SC.
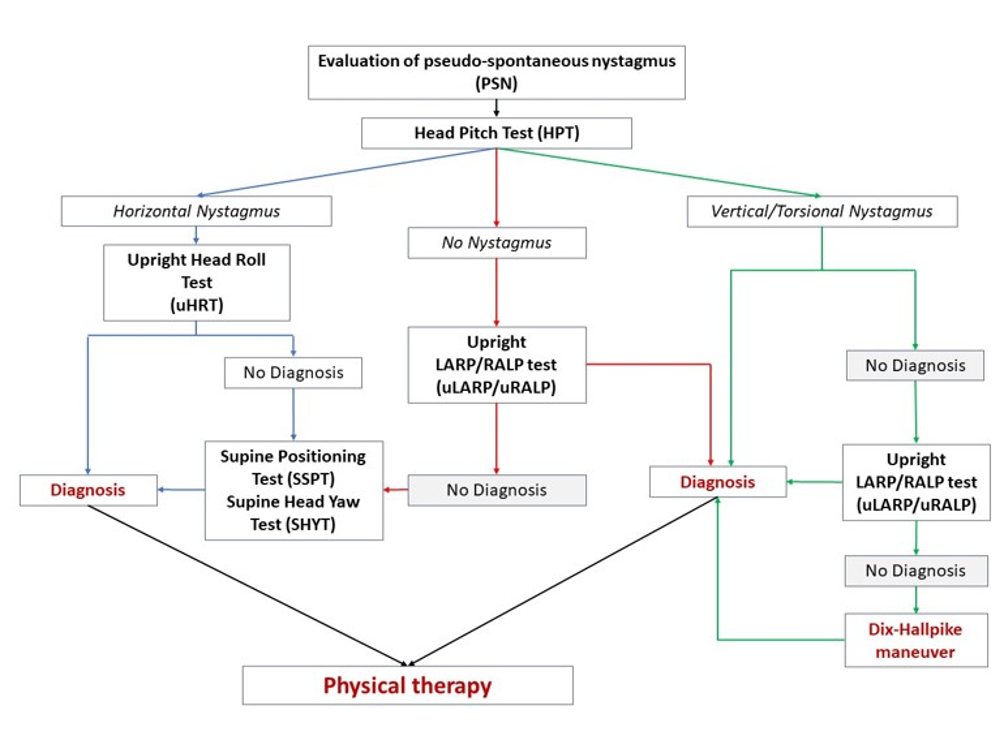
Figure 1. Diagnostic algorithm for BPPV according to the Minimum Stimulus Strategy (MSS) (from Asprella Libonati G, Martellucci S, Castellucci A, Malara P. J Neurol Sci. 2022).
In UBP each test has been properly named according to the spatial plane (roll, pitch and yaw plane) identified by the axis around which the head is rotated (X, Y and Z axis, respectively). Moreover, considering the spatial orientation of the vertical SCs, two additional planes aligned with each couple of vertical SCs can be described: left anterior – right posterior (LARP) and right anterior – left posterior (RALP).
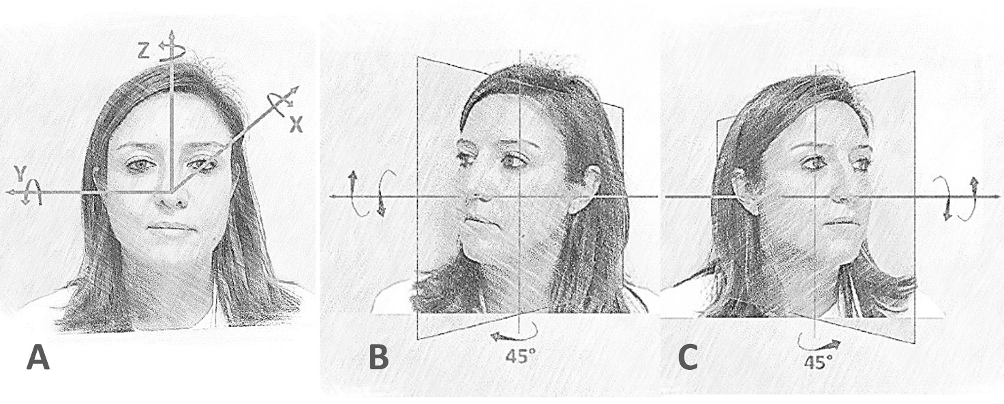
Figure 2. (A) Schematic overview of head rotations along the X, Y and Z axes. Left anterior – right posterior (LARP) (B) and right anterior – left posterior (RALP) canal planes (C) with corresponding head rotations (from Asprella Libonati G, Martellucci S, Castellucci A, Malara P. J Neurol Sci. 2022).
The first step of the UBP is the evaluation of pseudo-spontaneous nystagmus (PSN) in the primary gaze eyes position. Then, any patient with a history consistent with BPPV should be checked performing the upright head pitch test (uHPT) while sitting. PSN is a direction-changing nystagmus, which changes its beating direction according to the head bending angle. According to literature, over 50% of HSC-BPPV cases presents with PSN. Therefore, the uHPT (also called “Bow and Lean test”) represents the second step of the UBP. It is performed slowly bending the patient's head 60° forward and then 30° backward from the horizontal plane, turning the head around the X-axis (along the pitch plane). The head should be held still in both positions until nystagmus appears (usually within 30 s). The uHPT modifies the direction of any previously detected PSN, whereas the uHPT can elicit horizontal direction-changing nystagmus reversing according to the head bending angle in the case PSN is lacking. Conversely, the uHPT might evoke vertical nystagmus with variable torsional components in BPPV affecting vertical SCs. Therefore, the uHPT represents the turning point in the UBP algorithm.
Then, the upright Head Roll Test (uHRT) represents the third step of UBP and it is performed after positive HPT. Accordingly, the patient's head is slowly bent about 30° laterally towards each side, turning around the Z axis (along the roll plane) and bringing the patient's ear close to the shoulder of the same side. Even in this case, the head should be held still in each position until nystagmus appears (usually within 30 s). Once horizontal nystagmus (either geotropic or apogeotropic) is elicited, the same maneuver is performed towards the contralateral side to check if the nystagmus reverses the direction. According to the literature, the HSC-BPPV affected side and its variant (geotropic or apogeotropic) can be identified in over 90% of cases matching data obtained from UBP test battery, even if the above-mentioned upright tests give incomplete results. When UBP allows a reliable diagnosis of HSC-BPPV, it is suggested to proceed with the appropriate therapeutic maneuvers. Otherwise, it is mandatory to continue evaluating the nystagmus evoked by bringing the patient supine (seated-supine positioning test - SSPT) and performing the other positioning tests while supine (Supine Head Yaw Test - sHYT, also known as Supine Head Roll Test or Pagnini-McClure maneuver).
In BPPV affecting vertical SCs, the uHPT might evoke vertical nystagmus, either up-beating or down-beating, with torsional components. The uHPT in typical PSC-BPPV (also called geotropic variant) usually evokes a direction-changing nystagmus. Namely, down-beating nystagmus with torsional components towards the unaffected ear might be observed bending the patient's head forward, whereas opposite nystagmus (up-beating with rotational components towards the affected side) might be detected in backward head bending. Conversely, both head bending along the pitch plane, forwards and backward, might result in down-beating nystagmus in ASC-BPPV and apogeotropic form of PSC-BPPV, whereas torsional components might be less easily detectable. In these cases, the identification of the affected SC might be challenging, because torsional components might be lacking evoked performing the traditional positioning tests (i.e., Dix Hallpike maneuver, Semont maneuver, etc.). More recently, it has been demonstrated that the sensitivity of the UBP for the diagnosis of PSC-BPPV increases aligning the patient's head with the plane of the examined vertical SCs couple. The term upright LARP (uLARP) and upright RALP (uRALP) test has been adopted to describe the positioning maneuvers conducted along the left anterior – right posterior and right anterior – left posterior canal planes, respectively, with the patient in the sitting position. Right PSC-BPPV can be diagnosed performing the uLARP test by slowly bending the patient's head backward and forward along the LARP plane and, similarly, the involvement of the left PSC can be easily detected performing the uRALP test. Once the affected SC has been identified, it is possible to confirm the right diagnosis performing the ipsilateral Dix Hallpike or Semont maneuver, and then, finally, performing the therapeutic maneuvers.
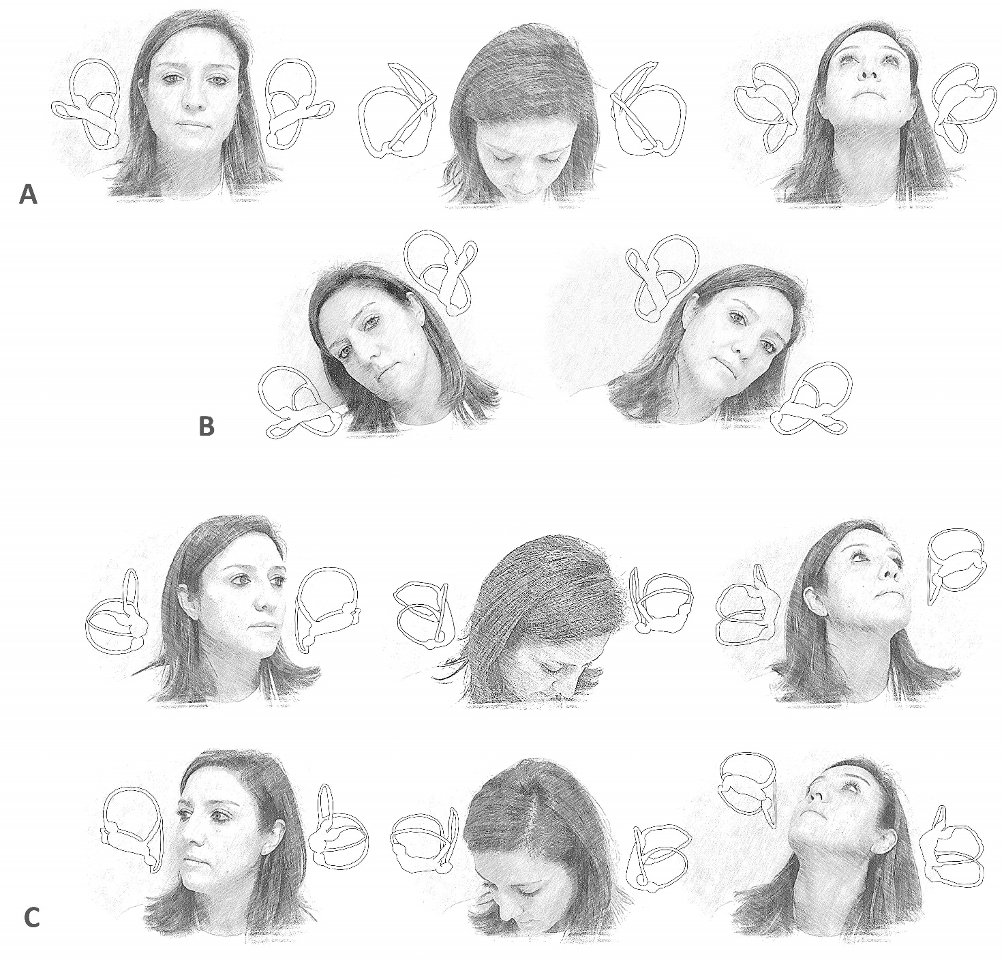
Figure 3. Upright BPPV protocol (UBP). (A) Upright Head Pitch Test (uHPT): the patient's head is bent forward and backward around the Y (interaural) axis and along the pitch plane. (B) Upright Head Toll Test (uHRT): the patient's head is tilted rightward and leftward around the X (naso-occipital) axis and along the roll plane. (C) uRALP/uLARP test: the patient's head is bent forward and backward along the RALP and LARP planes, respectively (from Asprella Libonati G, Martellucci S, Castellucci A, Malara P. J Neurol Sci. 2022).
AudiologyOnline: Which are the steps of the Minimum Stimulus Strategy in the diagnosis of PSC-BPPV?
Andrea Castellucci: The typical variant of PSC-BPPV, also known as geotropic variant, accounts for around 80% of all BPPV diagnosis. Although most patients report the first positional vertigo while getting up from bed, positional symptoms recur frequently, simply moving the head along the vertical planes. Therefore, most patients experience brief and recurrent short-lasting vertigo attacks (from 15 to 30 s) by flexing or extending the head while upright, while lying down on the bed or turning the head towards the affected side while supine, usually associated with autonomic symptom (i.e., nausea and vomiting). Geotropic PSC-BPPV is due to free-floating otoconia within the ampullary arm of the PSC modifying the acceleration sensitivity of the cupula, according to the canalolithiasis theory. The diagnosis of PSC-BPPV is traditionally achieved with the Dix-Hallpike or the Semont diagnostic maneuver, by detecting the typical positional nystagmus generated by an otoconial shift away from the cupula, thus resulting in an ampullofugal excitatory endolymphatic flow. It typically lasts less than 1 min and presents with up-beating and ipsilesional torsional components. The UBP algorithm allows the proper diagnosis of PSC-BPPV in most cases, particularly in recent-onset cases. The typical excitatory nystagmus (up-beating with torsional components towards the affected ear) is commonly observed bending the patient's head backward at the uHPT, whereas opposite inhibitory nystagmus (down-beating with torsional components towards the healthy side) can be observed in forward head bending. In the case the uHPT is ineffective and clinicians cannot detect any clear torsional components, the UBP diagnostic sensitivity is significantly increased moving the patients' head along the RALP and LARP planes, thus performing the uRALP and uLARP tests. Since the RALP plane approximately aligns with the left PSC, in the uRALP test the patient's head is rotated 45° to the left side from the neutral position and then bent 60° forward and 30° backward. In case of left PSC-BPPV, the uRALP test more easily induce either inhibitory or excitatory endolymphatic flows compared to the uHPT, since it moves the head along the plane of the affected canal resulting more effective in evoking either inhibitory (down-beating/right-torsional) or excitatory (up-beating/left-torsional) nystagmus. Conversely, uRALP should not detect any eye movements in case of right PSC-BPPV, as both head movements and the gravity vector axis align with a plane orthogonal to the right PSC plane, preventing any otoconial movements. Similarly, the uLARP test is conducted with the patient's head rotated 45° to the right side to align head bendings and gravity with the right PSC plane. In case of right PSC-BPPV, forward head bending elicits inhibitory down-beating/left-torsional nystagmus whereas backward head bending results in up-beating/right-torsional nystagmus. Accordingly, the uLARP is unable to detect any eye movements in case of left PSC-BPPV as both head movements and gravity axis align with a plane orthogonal to left PSC plane. Recently published data in typical PSC-BPPV has shown that a correct diagnosis can be achieved in 75.23% with the sole HPT and in 87.16% of cases adding uRALP/uLARP test. The diagnostic delay appeared closely related to the sensitivity of the UBP. Once the affected side has been identified, the diagnosis of PSC-BPPV should be confirmed with one of the traditional diagnostic tests (Dix-Hallpike or Semont maneuver).
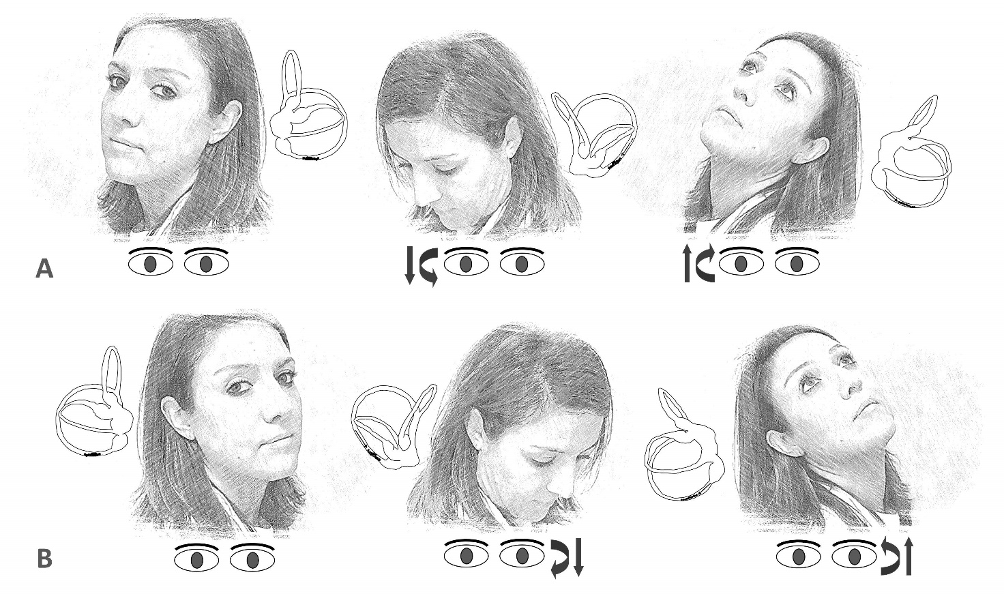
Figure 4. (A) uRALP test for the diagnosis of left PSC-BPPV. (B) uLARP test for the diagnosis of right PSC-BPPV. The arrows within the canal represent the direction of endolymphatic flows, whereas the arrows beneath the eyes represent the direction of the fast phase of nystagmus (from Asprella Libonati G, Martellucci S, Castellucci A, Malara P. J Neurol Sci. 2022).
AudiologyOnline: Which are the steps of the Minimum Stimulus Strategy in the diagnosis of HSC-BPPV?
Andrea Castellucci: HSC-BPPV is the second most common type of BPPV, accounting for 15–25% of all BPPV diagnosis. In this case, positional vertigo can be triggered by head movements along the HSC plane and are usually more severe than PSC-BPPV, as they are typically associated with stronger autonomic symptoms and last longer than 30 s. Patients usually experience the first acute vertigo attack when turning sideways in the bed. Nevertheless, subjects might have mild transient dizziness whenever head movements move otoliths within the affected HSC, e.g., bending or turning the head while sitting, or lying down supine and turning head on one side. The diagnosis of HSC-BPPV is usually obtained identifying the typical horizontal, direction-changing positional nystagmus evoked with the diagnostic maneuver known as “Supine Head Roll Test” or “McClure-Pagnini test”. Since it is conducted turning the head 180° to either side along the yaw plane while supine, the name Supine Head Yaw Test (sHYT) seems more correct.
In HSC-BPPV, nystagmus is purely horizontal, with variable directions according to the otoliths position within the affected HSC. Two forms of HSC-BPPV can be identified, depending on the direction of the nystagmus evoked by the sHYT:
- The geotropic form is due to debris floating along the non-ampullary arm of the HSC (“geotropic canalolithiasis”).
- The apogeotropic form is due either to debris attached to the cupula (“cupulolithiasis”) or to free-floating particles within the ampullary arm of the canal (“apogeotropic canalolithiasis”).
The diagnosis of the affected side by the sHYT is based on comparing the nystagmus intensity evoked on each side in accordance with Ewald's second law, postulating that the response to an excitatory stimulus, due to ampullopetal deflection of the HSC cupula, is always stronger than following an inhibitory stimulus, due to ampullofugal deflection. The affected side is the one where the nystagmus is stronger in geotropic variant, whereas the involved ear is the side where the nystagmus is weaker in apogeotropic form. The nystagmus intensity difference in performing the sHYT is sometimes hardly detected. In these cases, checking the patients more times by repeated repositioning tests could result in significant discomfort due to severe autonomic symptoms, especially in phobic and anxious subjects or in patients with recent onset of BPPV, thus preventing the proper diagnosis and treatment. The UBP protocol allows to avoid such complications. The evaluation of PSN represents the first step of UBP. The HSC works as an inclined surface drawing a 30° front-open-angle with the horizontal plane, either allowing free-floating particles to gravitate along the canal (in canalolithiasis) or resulting in a persistent displacement of the heavy cupula (in cupulolithiasis). Therefore, the PSN, if detected, is generally directed to the healthy side in geotropic forms, as debris float away from the ampulla, and to the affected side in apogeotropic variants, as particles move towards the ampulla. Bending the head backward at the uHPT, the angle between the HSC and the horizontal plane increases either enhancing PSN amplitude, if detectable, or eliciting nystagmus beating towards the healthy side in geotropic forms and towards the affected side in apogeotropic variants. Otherwise, PSN disappears when the head is bent 30° forward (neutral position) as the HSC aligns with the horizontal plane, while it reverses when the head is further bent forward. In case PSN is not detectable in primary position, forward head bending should elicit nystagmus beating to the affected side in geotropic variant and towards the healthy side in apogeotropic form. Therefore, the uHPT allows clinicians to restrict the diagnostic hypotheses to two sole options: the geotropic variant of one HSC or the apogeotropic variant involving the HSC of the opposite side. Nevertheless, it does not allow to distinguish between these two. In this situation, the correct diagnosis can be achieved with the uHRT. In fact, head bending towards each side allow gravity to move debris within the involved HSC eliciting positional nystagmus. This latter could be directed on both sides: either towards the undermost ear in the geotropic form or towards the uppermost ear in the apogeotropic one. Therefore, the correct detection of the affected side and the involved canal arm of the HSC can be simply achieved combing the data provided by both upright tests: uHPT and uHRT. For example, in case of canalolithiasis of the non-ampullary arm of the right HSC (i.e., right geotropic HSC-BPPV), the PSN, if detectable, should beat to the left side, whereas the uHPT should result in right-beating nystagmus in forward head bendings and left-beating nystagmus in head extensions. Finally, the uHRT should likely result in left-beating (geotropic) nystagmus in leftward head tilts and in right-beating (still geotropic) nystagmus in rightward head tilts. Conversely, in case of right apogeotropic HSC-BPPV either due to cupulolithiasis or to ampullary arm canalolithiasis, PSN, if detectable, should be directed rightward similarly to the nystagmus induced in backward head bending at the uHPT, whereas forward head flexions should result in left-beating nystagmus. Finally, the uHRT should provide the correct diagnosis leading to apogeotropic nystagmus tilting the head on both sides along the roll plane. In case of incomplete responses, it can be suggested to apply some slight inertial accelerations to the patient's head, to facilitate otoconial floating along the HSC with uHPT and uHRT. According to the literature, a correct diagnosis for HSC-BPPV can achieved in over 95% of cases using exclusively the UBP, regardless of the time elapsed from symptoms onset to diagnosis.
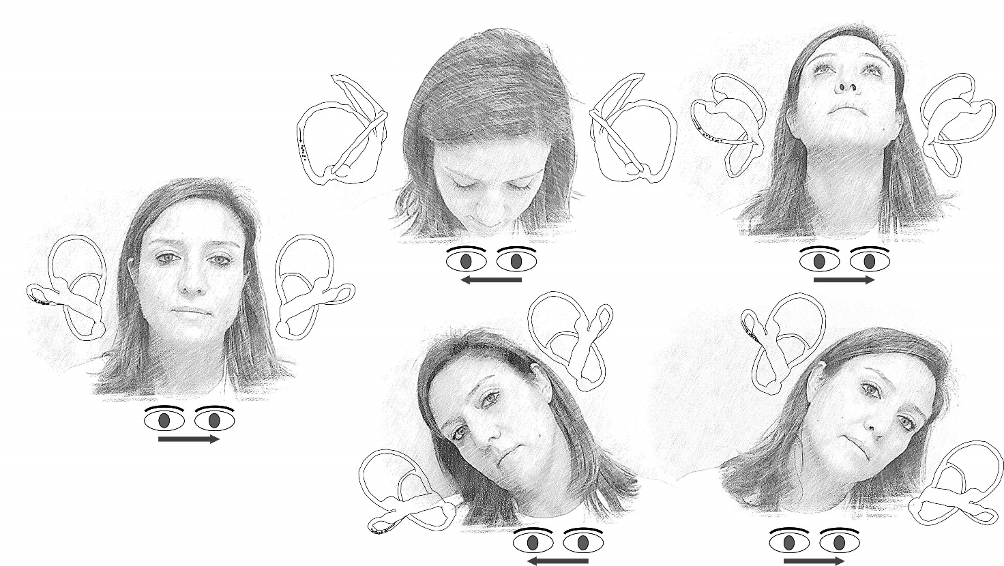
Figure 5. UBP for right geotropic HSC-BPPV. The arrows within the canal represent the direction of endolymphatic flows, whereas the arrows beneath the eyes represent the direction of the fast phase of nystagmus (from Asprella Libonati G, Martellucci S, Castellucci A, Malara P. J Neurol Sci. 2022).
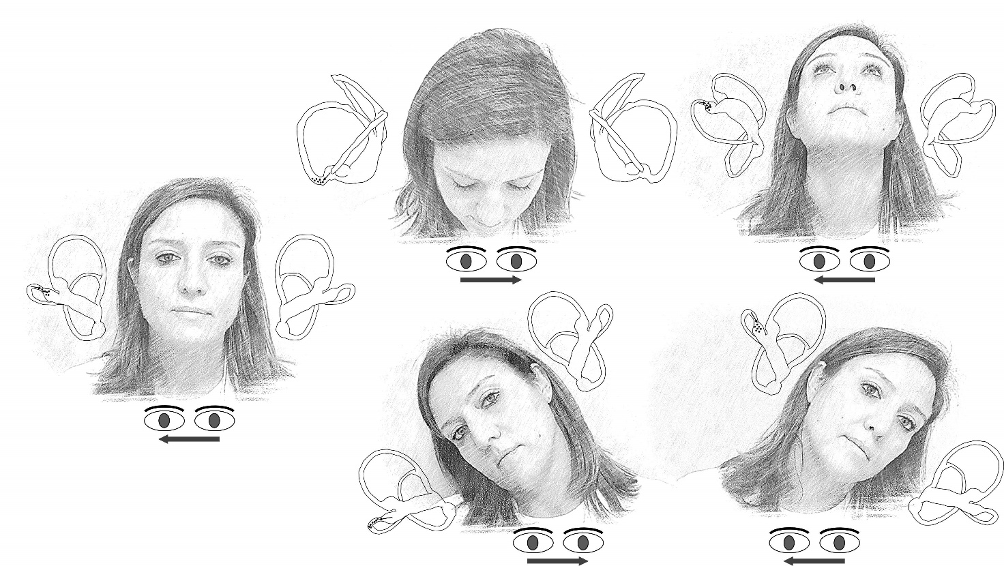
Figure 6. UBP for right apogeotropic HSC-BPPV. The arrows within the canal represent the direction of endolymphatic flows, whereas the arrows beneath the eyes represent the direction of the fast phase of nystagmus (from Asprella Libonati G, Martellucci S, Castellucci A, Malara P. J Neurol Sci. 2022).
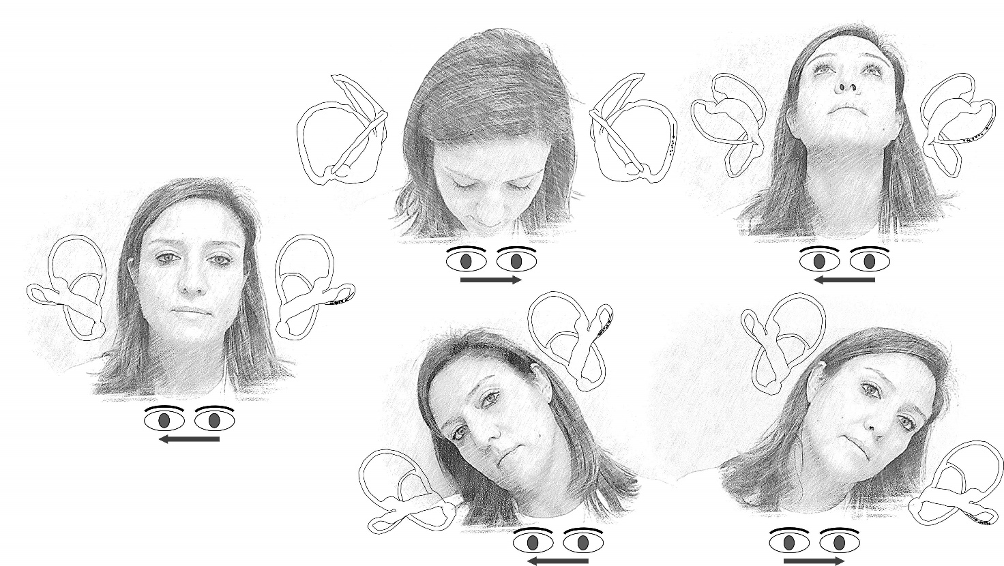
Figure 7. UBP for left geotropic HSC-BPPV. The arrows within the canal represent the direction of endolymphatic flows, whereas the arrows beneath the eyes represent the direction of the fast phase of nystagmus (from Asprella Libonati G, Martellucci S, Castellucci A, Malara P. J Neurol Sci. 2022).
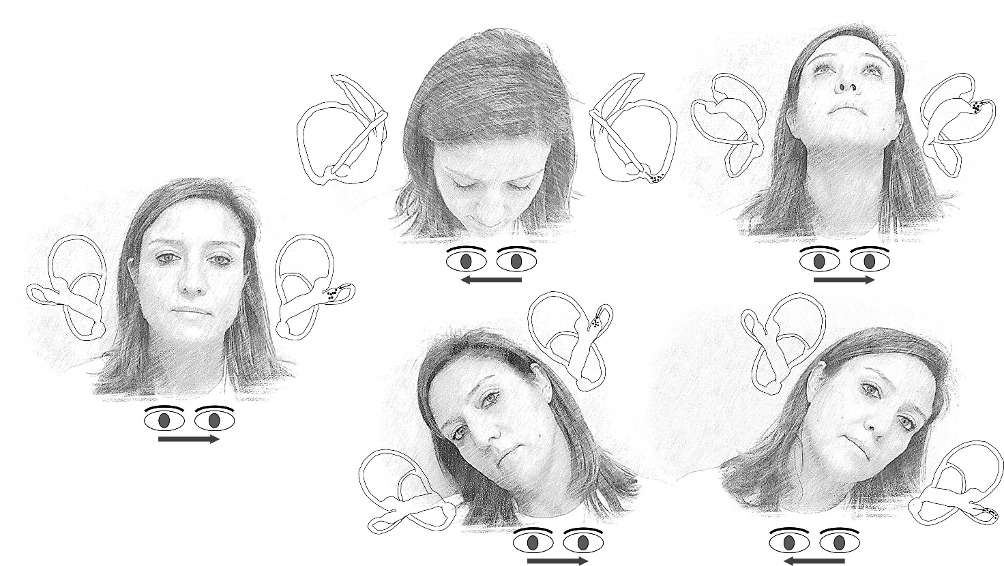
Figure 8. UBP for left apogeotropic HSC-BPPV. The arrows within the canal represent the direction of endolymphatic flows, whereas the arrows beneath the eyes represent the direction of the fast phase of nystagmus (from Asprella Libonati G, Martellucci S, Castellucci A, Malara P. J Neurol Sci. 2022).
In the case of ineffective UBP, other secondary signs of lateralization, such as the evoked nystagmus at the SSPT, should be sought. This nystagmus can be evoked bringing the patient supine from the sitting position along the pitch plane. In this position, the HSC aligns with the gravity vector and otoliths gravitate along the involved HSC arm. Therefore, in geotropic variants, debris float away from the ampulla along the non-ampullary arm leading to an inhibitory endolymphatic flow resulting in contralesional nystagmus. Otherwise, in apogeotropic variants, either particles float towards the cupula along the ampullary arm (in canalolithiasis) or the heavy cupula bends ampullopetally (in cupulolithiasis); in both cases SSPT results in excitatory stimulus and in ipsilesional nystagmus. Once nystagmus evoked at the SSPT has been detected, the sHYT is performed turning the patient's head 180° to either side
AudiologyOnline: Which are the steps of the Minimum Stimulus Strategy in the diagnosis of ASC-BPPV or apogeotropic PSC-BPPV resulting in positional down-beating nystagmus?
Andrea Castellucci: Positional down-beating nystagmus (pDBN) represents one of the most common findings related to central nervous system disorders involving the brainstem and cerebellum and usually present purely vertical direction, long duration, lack of latency, fatigability, and no suppression with visual fixation. Nevertheless, it has been widely demonstrated how pDBN may also occur in peripheral pathologies including ASC-BPPV and a recently described variant of PSC-BPPV known as apogeotropic PSC-BPPV (aPSC-BPPV). In this latter form, it has been hypothesized that otoliths settle in the distal portion of the non-ampullary tract of the PSC so that it is named “apogeotropic variant”, as nystagmus evoked in provoking positions beats away from the ground and in the opposite direction to positional paroxysmal upbeat nystagmus due to classical PSC-BPPV. An intensity-variable vertical down-beating can be elicited in both forms when the patient is brought into the straight head hanging (SHH) position and by Dix-Hallpike test. pDBN associated with BPPV usually lacks of paroxysm, clear torsional components and direction reversal in returning to the sitting position. The same oculomotor features can also be observed at the UBP: down-beating nystagmus can be elicited at the HPT by bending the patient's head forward or backward, while uRALP/uLARP test can sometimes facilitate the recognition of torsional components, similarly to MSS applied to PSC-BPPV.
References
Asprella Libonati G, Gagliardi G, Cifarelli D, Larotonda G (2003). “Step by step” treatment of lateral semicircular canal canalolithiasis under videonystagmoscopic examination. Acta Otorhinolaryngol Ital, 23:10–15.
Asprella Libonati G (2005). Diagnostic and treatment strategy of lateral semicircular canal canalolithiasis, Acta Otorhinolaryngol Ital. 25:277–283.
Asprella Libonati G (2008). Pseudo-spontaneous nystagmus: a new sign to diagnose the affected side in lateral semicircular canal benign paroxysmal positional vertigo. Acta Otorhinolaryngol Ital. 28:73–78.
Asprella Libonati G, Martellucci S, Castellucci A, Malara P (2022). Minimum Stimulus Strategy: A step-by-step diagnostic approach to BPPV. J Neurol Sci, 434:120158.
Bhattacharyya N, Gubbels SP, Schwartz SR, et al. (2017). Clinical practice guideline: benign paroxysmal positional vertigo (Update), Otolaryngol. Head Neck Surg, 156 (3_suppl):S1–S47.
Califano L, Melillo MG, Mazzone S, Vassallo A (2010). “Secondary signs of lateralization” in apogeotropic lateral canalolithiasis. Acta Otorhinolaryngol Ital, 30:78–86.
Choi S, Choi HR, Nahm H, Han K, Shin JE, Kim CH (2018). Utility of the bow and lean test in predicting subtype of benign paroxysmal positional vertigo, Laryngoscope, 128:2600–4.
Choo OS, Kim H, Jang JH, Park HY, Choung YH (2020). Vertical nystagmus in the Bow and lean test may indicate hidden posterior semicircular canal benign paroxysmal positional vertigo: hypothesis of the location of otoconia. Sci Rep, 10:6514.
Choung YH, Shin YR, Kahng H, Park K, Choi SJ (2006). “Bow and lean test” to determine the affected ear of horizontal canal benign paroxysmal positional vertigo. Laryngoscope, 116:1776–81
Im DH, Yang YS, Choi H, Choi S, Shin JE, Kim CH (2017). Pseudo-spontaneous nystagmus in horizontal semicircular canal canalolithiasis. Medicine 96:e7849.
Koo JW, Moon IJ, Shim WS, Moon SY, Kim JS (2006). Value of lyingdown nystagmus in the lateralization of horizontal semicircular canal benign paroxysmal positional vertigo, Otol Neurotol, 27:367371.
Lee HJ, Kim YH, Hong SK, Kim HJ (2012). Pseudo-spontaneous nystagmus in lateral semicircular canal benign paroxysmal positional vertigo. Clin Exp Otorhinolaryngol, 5:201–206.
Lee JB, Han DH, Choi SJ, et al (2010). Efficacy of the “bow and lean test” for the management of horizontal canal benign paroxysmal positional vertigo. Laryngoscope, 120:2339–46.
Lee SH, Choi KD, Jeong SH, Oh YM, Koo JW, Kim JS (2007). Nystagmus during neck flexion in the pitch plane in benign paroxysmal positional vertigo involving the horizontal canal. J Neurol Sci, 256:75–80.
Lee SU, Kim HJ, Kim JS (2014). Pseudo-spontaneous and head-shaking nystagmus in horizontal canal benign paroxysmal positional vertigo. Otol Neurotol, 35:495–500.
Malara P, Castellucci A, Martellucci S (2020). Upright head roll test: A new contribution for the diagnosis of lateral semicircular canal benign paroxysmal positional vertigo. Audiol Res, 10(1):236.
Marcelli V (2016). Nystagmus intensity and direction in bow and lean test: an aid to diagnosis of lateral semicircular canal benign paroxysmal positional vertigo. Acta Otorhinolaryngol Ital, 36:520–6.
Martellucci S, Malara P, Castellucci A, et al (2020). Upright BPPV Protocol: Feasibility of a New Diagnostic Paradigm for Lateral Semicircular Canal Benign Paroxysmal Positional Vertigo Compared to Standard Diagnostic Maneuvers. Front Neurol, 11:578305.
Martellucci S, Castellucci A, Malara P, et al (2022). Is it possible to diagnose Posterior Semicircular Canal BPPV from the sitting position? The role of the Head Pitch Test and the upright tests along the RALP and LARP planes. Am J Otolaryngol, 43(4):103474.
Nuti D, Masini M, Mandalà M (2016). Benign paroxysmal positional vertigo and its variants. Handb Clin Neurol, 137(137):241–256.
Scarpa A, Cassandro C, Gioacchini FM, et al (2019). Lateralization of horizontal semicircular canal benign paroxysmal positional vertigo (HSC-BPPV) with the latency test: a pilot study. Acta Otolaryngol, 139(10):854-9.
Yetiser S, Ince D (2015). Diagnostic role of head-bending and lying-down tests in lateral canal benign paroxysmal positional vertigo. Otol Neurotol, 36:1231–7.
Resources for More Information
For more information, visit https://www.inventis.it/en-na


