From the Desk of Gus Mueller
 The early 1970s were an exciting time for diagnostic audiology. In addition to the first published work on the human ABR, we had this new test—immittance audiometry—introduced to our clinics (although it wasn’t dubbed “immittance” until several years later). While electronic impedance equipment had been around in Europe for a decade or more, it was not until 1968 that a clinically friendly model, the Madsen ZO-70 “bridge”, was introduced in the U.S. James Jerger, who was at Baylor College of Medicine at the time, received one the first units, and in 1970 he published his findings for his center’s first 400 patients. The intriguing equipment and test procedures, coupled with the supporting documentation from Jerger, caught the attention of most all clinicians. The topic of “how the heck do you get a good seal” soon replaced talk of Békésy types and ABLB ladder-grams at late-night audiology gatherings.
The early 1970s were an exciting time for diagnostic audiology. In addition to the first published work on the human ABR, we had this new test—immittance audiometry—introduced to our clinics (although it wasn’t dubbed “immittance” until several years later). While electronic impedance equipment had been around in Europe for a decade or more, it was not until 1968 that a clinically friendly model, the Madsen ZO-70 “bridge”, was introduced in the U.S. James Jerger, who was at Baylor College of Medicine at the time, received one the first units, and in 1970 he published his findings for his center’s first 400 patients. The intriguing equipment and test procedures, coupled with the supporting documentation from Jerger, caught the attention of most all clinicians. The topic of “how the heck do you get a good seal” soon replaced talk of Békésy types and ABLB ladder-grams at late-night audiology gatherings.
It was not long after the ZO-70 impedance bridge arrived that the Grason-Stadler company came out with their Model 1720 admittance unit. Confusion ensued. Were we measuring impedance or admittance? Ohms or mhos? Were we using a bridge or a meter?

Gus Mueller
It was also about this time that a road show, nearly as popular as today’s Diners, Drive-Ins and Dives, was launched. Irwin Klar, a New York distributor of audiometric equipment, put together a traveling “educational event” to teach clinicians about this new and exciting diagnostic procedure. The lead instructor was Jerry Northern, with noted regular guest speakers, the likes of Jim Jerger, Chuck Berlin, Bob Keith and Laura Wilbur. These workshops were held in dozens of U.S. cities, usually to a packed house of clinicians wanting to learn about this new technology. Klar soon came out with his own impedance equipment, the American Electromedics. Some of you might remember the automatic pediatric tympanometry unit which also was soon available from this company, which had the novel idea of having a car printed on the recording paper, that then moved when a seal of the ear canal was obtained. A great distraction for a squirming kid.
Okay, enough history. That was the world of immittance audiometry from the 1970s, but what about now? We of course still do tympanograms and acoustic reflex measures, but do they still have the diagnostic weight that they did then? And what is new? Things must have changed in 40 years?
To answer all these questions, we have our 20Q guest author, Lisa L. Hunter, PhD, Scientific Director for Audiology in the Communication Sciences Research Center at Cincinnati Children’s Hospital Medical Center, and Associate Professor of Otolaryngology and Communication Sciences and Disorders at the University of Cincinnati. You’re probably familiar with the many publications from Dr. Hunter on otitis media, pediatric audiology and diagnostic audiology. She also is the principle investigator of a large NIH project on Newborn Hearing Screening and Diagnosis.
Dr. Hunter is a graduate and former faculty member of the University of Minnesota and in the early 2000s she developed and directed the AuD program at the University of Utah. Lisa has chaired numerous committees for national professional organizations and currently is a member of the Board of Directors of the Accreditation Commission for Audiology Education. She also served on the American Academy of Audiology's Board of Directors for many years.
This 20Q is just a glimpse of Dr. Hunter’s expertise in the area of immittance audiometry. For those of you who’d like more, check out her recently released textbook on the topic titled: Acoustic Immittance Measures—Basic and Advance Practice from Plural Publishing.
Gus Mueller, Ph.D.
Contributing Editor
September 2013
To browse the complete collection of 20Q with Gus Mueller articles, please visit www.audiologyonline.com/20Q
20Q: Acoustic Immittance - What Still Works & What's New

Lisa Hunter
1. Clinical immittance testing has been around a long time, hasn’t it?
Relatively speaking, yes. Even before I was born! There are reports of acoustic reflex testing using an impedance bridge going back to Otto Metz in Denmark in 1946. You may have heard of or read the classic papers by Jerger in early 1970s, and later by Green and Margolis (1984) and Gelfand (1984) where the different acoustic reflex patterns were explained, illustrating how they might be used for clinical diagnosis of different pathologies. Tympanometry, as we know it today, was introduced by some other Danish researchers, Terkildsen and Scott-Nielsen in 1957 who developed the first pressurized acoustic immittance instrument, the Madsen ZO61. Now that was a fine piece of hardware, all polished wood and heavy metal! The patterns we often refer to today were first described by Lidén (1969) and Jerger (1970).
2. Okay, that’s what I thought. Much of what we do today has been around for over 50 years. But I keep thinking that there must be some changes and clinical refinements that have been made since I was in graduate school?
There definitely have been, and these advances are now available commercially. It’s true that you could do the basic immittance battery of today using the equipment that we had in in our clinics in the early 1970s, but we certainly have made some advances in instrumentation and how we interpret the findings.
3. Okay, I’m here to learn. Let’s start with the tympanogram. I was taught to classify them into five types—A, B, C, AS and AD. Is that still okay?
Typing tympanograms is a nice, easy to remember system and was used from the 1960’s when instruments weren’t calibrated as precisely as they are today. Those early instruments didn’t provide quantified measurements – just a shape was all we had to work with. That’s pretty much like measuring height with “short, medium and tall”. During the 1980’s, most instruments were finally calibrated and provided at least a measure of admittance (peak height) that could be quantified. Typing by shape is about 60-70% sensitive – not all that great – who wants to miss 30-40% of middle ear fluid cases? Measuring the width (at 50% of the peak height) boosts the sensitivity to about 80%, which is not perfect but much better. So, for detecting OME or other problems that increase stiffness of the system, add width to your measurements. Norms for tympanometry measures are available for infants, children and adults in Table 1, which is averaged from studies reviewed in Hunter and Shahnaz (2013).
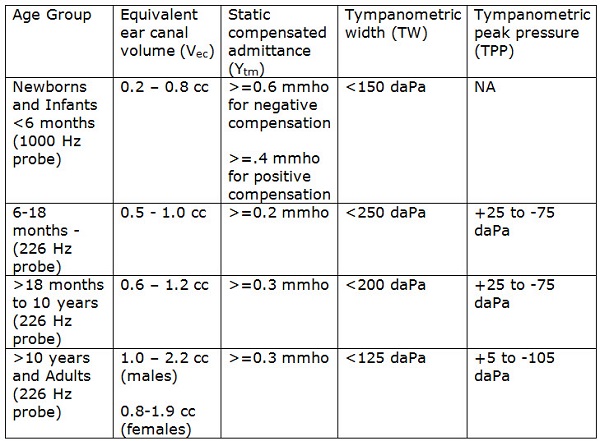
Table 1. Normative measures for tympanometry, compiled from multiple studies reviewed in Hunter and Shahnaz, 2013.
4. I have to admit I haven’t been using width calculations. How do you report these findings to the referring physician?
An overall normal or abnormal interpretation is the clearest way to report to a physician, and it is fine to use A, B, C etc. typing as long as you know the age-appropriate normal ranges. The tympanogram width is abbreviated TW, and is reported in decaPascals (daPa). This should be interpreted in addition to static admittance in mmho, equivalent volume in cc, and peak pressure in daPa. Here’s an example of what you might say:
5. Thanks—that helps. I get a lot of requests to do tympanometry on newborns and infants. I’ve heard, however, that it isn’t very accurate with that population. Is there any other test I can use instead?
You don’t really need a new test—just modify the one you’ve been using. It isn’t really tympanometry that’s the problem here, it’s the reliance on our good old 226-Hz probe tone that’s the issue. Low-frequency tympanometry assumes that you are measuring in a hard-walled cavity (the ear canal). Newborns and infants up to about 6 months old have hyper-mobile ear canals because the bones in the ear canal wall haven’t ossified yet. So the low-frequency sound energy gets absorbed by those super-compliant tissues. If the middle ear is chock-filled with fluid, you will still get a peaked tympanogram because it’s the ear canal responding to the pressure changes rather than the middle ear system. So what’s an audiologist to do? Just crank up that probe frequency to 1000 Hz, which fortunately isn’t as affected by the compliant ear canal, and you can still do tympanometry in those babes. Norms are available from Margolis and colleagues (2003) or Kei et al. (2003), as shown in Table 1. Better yet, you can use wideband absorbance – a new test that appears to be even more sensitive and specific than tympanometry in newborns.
6. You just lost me . . . absorbance?
Right. A new way to measure middle ear function is called wideband reflectance or absorbance, or if pressurized, is known as 3D wideband tympanometry. An example is shown in Figure 1. These tests are entirely different from an instrument known as “reflectometry”, which is a hand-held screening test of the time delay in sound coming back from the eardrum. Reflectometry is not as sensitive as tympanometry, so it is not recommended as a diagnostic measure. In contrast, wideband absorbance measures sound energy absorbed by the eardrum and middle ear. It uses clicks, and can analyze how sound is absorbed from 200 Hz up to about 10,000 Hz. It can be done with pressure, just like tympanometry, which then gives us 3 dimensions. Wideband acoustic reflexes can also be measured with this technique. So far, results are very promising in studies for infants, children and adults. An entire edition of Ear and Hearing (2013, Supplement 1) was just published that provides many articles from experts in this new exciting area of diagnostic testing.
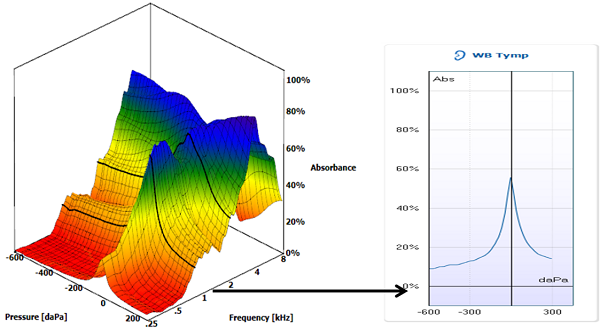
Figure 1. A wideband tympanogram and an averaged tympanogram between 1-4 kHz, showing how they relate to one another. This was recorded in a normal ear using the Interacoustics Titan (Denmark).
7. Sounds intriguing, but I’m guessing this means I’ll need to buy new equipment to do the testing?
Yes, in order to use the new absorbance technology, new equipment is necessary. There are instruments available that are combined with OAEs from Interacoustics, which are pressurized and include the 3D tympanograms, and Mimosa Acoustics, which tests wideband reflectance and absorbance at ambient pressure. Both wideband instruments are now FDA approved. They can provide more sensitive results for a wide range of pathologies such as idiopathic conductive or mixed hearing loss, suspected otosclerosis, ossicular disarticulation, OME, and other middle ear problems. The test is more sensitive because the entire audiometric frequency range is assessed by employing clicks with sophisticated calibration and analysis.
8. Getting back to traditional tympanometry, are Eustachian tube function tests used anymore, and are they accurate?
One basic measure of Eustachian tube (ET) function is the peak of the tympanogram, known as tympanometric peak pressure, or TPP. If the peak is within a normal range (+25 to -100 daPa), then the patient is able to adequately ventilate the middle ear during normal conditions (atmospheric pressure conditions). Some patients may complain of hearing their own voices, or “autophony”, which may indicate an abnormally open or patulous ET. Other patients may complain of ear pain or discomfort, especially during conditions that require active ET opening, such as airplane take-offs or landings, or diving. ET dysfunction is related to acute or chronic otitis media, especially in children. Detection of these problems is the main reason for doing ET function tests, such as measuring changes with Toynbee or Valsalva maneuvers, or after swallowing or sniffing. All of these maneuvers should result in opening of the ET and shifts in TPP. In patients with patulous ETs, 75% show fluctuations in admittance during breathing McGrath & Michaelides (2011). Studies of ET function tests have shown that these tests can tell you if the ET can open under active maneuvers, but they do not accurately predict patients who will have future OME problems (Straetemans et al. 2005).
9. So if I have a patient with any of the complaints you mention, you’re saying that I should routinely test ET function?
To detect a patulous ET, you can look for pulsatile admittance changes on the tympanogram or during reflex testing. ET function testing can be tried, and used to confirm whether the patient can open the ET actively. Just remember that it has no prognostic value to predict OME. It also would not provide value for treatment beyond what is gleaned from tympanometry.
10. One last question about tympanometry. It seems like it is being done by all kinds of providers, such as nurses in general practice offices and even hearing aid dispensers. Shouldn’t it only be done by audiologists?
Questions like this pop up on listservs all the time, and really make us sigh, navel gaze and wonder if we still matter. Are we defined by the tests we do, or by our intellectual input into these tests? Hearing and middle ear screening tests have been conducted by many non-audiologists for many years, and we could counter-argue that these efforts actually help our profession more than hurt us. Personally, I think we should encourage the ethical and responsible use of screening tests by physicians, nurses, speech pathologists and dispensers to identify and refer patients for appropriate care by audiologists and otolaryngologists. Such screening tests can identify patients for further assessment, ensure that patients with potentially treatable conditions such as cerumen impaction and middle ear problems receive medical care prior to hearing aid dispensing, and can increase recognition that an audiologist provides a higher level of care than just doing an audiogram or tympanogram. We should train and use support personnel to do screening tests whenever possible so that we can use our valuable time to provide more in-depth testing, counseling and treatment, thereby increasing the impact of audiology in ways that matter most.
11. I agree. I hope my career will not be defined by my ability to do a tympanogram. Let’s move on to acoustic reflex measures. Am I correct in saying that we still use these measures to help identify retro-cochlear pathology?
Yes. But if you want to have reasonable sensitivity and specificity, it’s important to use appropriate cut-off values. For example, 500 and 1000 Hz have normal cut-offs of 95 dB HL up to 50 dB HL hearing level, while 2000 Hz has a normal cut-off of 100 dB HL up to 45 dB of hearing loss. A table showing normal acoustic reflex thresholds by frequency and degree of hearing loss can be found in Gelfand, Schwander, and Silman (1990), and has been adapted in Table 2. There also is a chart in many textbooks such as shown in Table 3 that shows reflex results for various disorders, from the middle ear to the cochlea, on up to retrocochlear, including VIII nerve pathology, VII nerve and brainstem pathology. Understanding reflex test results is kind of like pattern recognition. The chart helps you figure out why the reflex can be absent in one ear and present in the other ear, or absent with the stimulus in one ear and present with the probe in that same ear. Understanding reflex pathways helps you figure out why these patterns happen – they are not random! In the case of a right-sided retrocochlear pathology, the reflex is elevated or absent (depending on size and location of the lesion) when the stimulus is delivered to the affected right ear. Contrast this pattern with a right-sided VII nerve lesion, in which the reflex is absent when it is measured with the probe in the affected right ear.
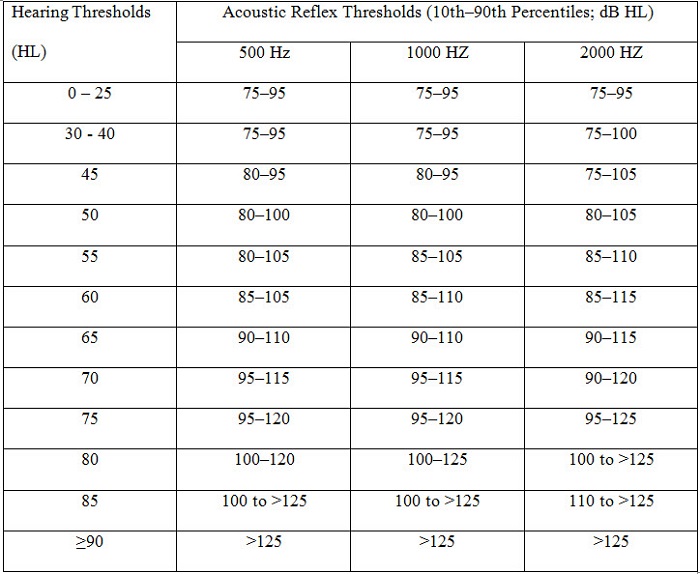
Table 2. Normative values for acoustic reflex thresholds (modified from Gelfand, Schwander, & Silman, 1990).
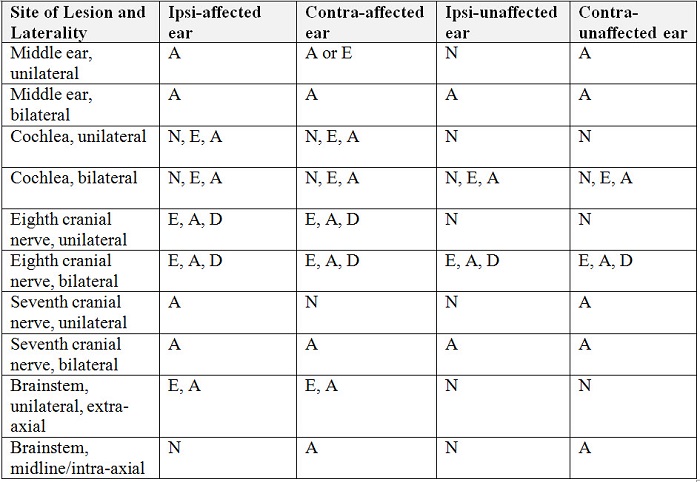
Table 3. Patterns of reflex abnormalities, referenced to the stimulus ear (modified from Hunter and Shahnaz, 2013). A = absent; E = elevated; N = normal; D = decay. Results that are variable depend upon severity of the condition or hearing loss.
12. I’ve heard that when you do contralateral reflexes, it’s debatable whether you report the reflex results for the stimulus ear or the probe ear?
No, it’s not debatable at all. There is only one correct way. You report for the ear that is stimulated. Granted, it might be confusing to a physician that a kid with left middle ear effusion has absent reflexes for the right ear, but that’s the way it is. The chart we just talked about makes it obvious which is the stimulus ear and which is the probe ear, so it should all be crystal clear!
13. Got it—it’s locked in. Is it true that if you do ipsilateral reflexes, there really is no reason to do contralateral?
Well, it depends on the situation. If I wanted to do a cross-check to confirm behavioral results, OAE or ABR in infants or children, I’d be satisfied with ipsilateral reflexes. Tympanometry is a better choice to rule out conductive hearing loss. Unilateral retrocochlear or facial nerve issues are rare in infants and children. Ipsilateral reflexes will give an answer regarding the possibility of cochlear loss or auditory neuropathy, combined with OAE and ABR. However, in working up new cases of hearing loss in children or adults and in complex or unclear cases at any age, contralateral reflexes are needed. In suspected neural involvement, and in working up cases of sensorineural hearing loss of unclear origin, both ipsilateral and contralateral reflexes are often helpful. Starting with ipsilateral reflexes, and continuing on to contralateral if ipsilateral reflexes are abnormal or do not fit the other results is a good back-up plan. And, there certainly are neurologic conditions such as multiple sclerosis or myasthenia gravis, where contralateral reflexes may be elevated, or delayed in latency, when both right and left ipsilateral look good.
14. What about when I have bilateral flat tympanograms - any reason to do reflex testing then?
Acoustic reflexes will nearly always be absent in this case, and assuming the probe is not blocked or against the ear canal wall and fits the overall pattern, you’ve got your answer. I’d be more interested in seeing how the tympanogram looked at higher frequencies, since 226 Hz alone doesn’t tell me what’s happening across the audiometric range, and so is a blunt tool.
15. So when I conduct either contralateral or ipsilateral reflex testing, should I test at 4000 Hz?
Let me first say that 4000 Hz is an overly sensitive reflex. Gets its feeling hurt often. What I mean is that even in normal-hearing ears, it is sometimes absent, it is smaller in amplitude, and shows a greater degree of decay. By far, 500, 1000 and 2000 Hz are better choices. 4000 Hz doesn’t add anything diagnostically, so you can save some time by doing one or more of the lower frequencies and adding contralateral recordings.
16. I’m all about not doing testing that isn’t diagnostically useful. And on that topic, now and then I read on audiology list serves that people are doing reflex decay testing. I thought we tossed that test out because of poor sensitivity/specificity years ago?
I’m never one to throw the baby out with the proverbial bathwater, and I still use reflex latency and decay judiciously, in suspected neurologic cases. But, it is true that acoustic reflex decay isn’t nearly as sensitive as an ABR, or certainly an MRI, for detecting retrocochlear pathology. The same of course can be said for our high-level word recognition measures, so many audiologists have dispensed with these classic site-of-lesion tests. The presence of high frequency hearing loss asymmetry greater than 15 dB has been shown to be more sensitive and specific than reflex decay or WR rollover testing, especially for small acoustic neuromas. Another consideration is that there have been some reports that reflex decay testing can cause noise-induced hearing loss (Hunter, Ries, Schlauch, Levine, & Ward, 1999) or tinnitus (Emanuel, Henson, & Knapp, 2012) if presented at high levels e.g., greater than 105 dB HL, so it’s best to limit testing below this level (Hunter et al. 1999). Additionally, if thresholds are elevated beyond the normal cut-off values, then the test is indicative of retrocochlear pathology already, so there is no need to add reflex decay testing, and no need to risk high level exposure.
17. So let’s say you do the decay testing and you get a positive finding. Does that then trigger an MRI?
Acoustic reflex decay combined with asymmetric sensorineural hearing loss is a strong reason to continue on to an MRI, and should provide the referring physician with the evidence needed to do the more expensive test. Since acoustic neuromas are fairly slow growing, depending on the age of the patient and history of noise exposure, the physician and patient may opt to monitor hearing if the acoustic reflexes are normal.
18. Is there any other good use for acoustic reflexes that we haven't discussed?
I have seen patients on a number of occasions who have functional hearing loss (pseudohypacusis) or were exaggerating hearing loss in both ears. A few times, these patients had fooled audiologists because they were so good at feigning a moderate or severe bilateral hearing loss for both pure tones and speech. One rule of acoustic reflex thresholds is that they cannot occur less than 20-25 dB above the pure tone threshold for 500, 1000 and 2000 Hz. This rule works very well for hearing thresholds between 60 and 90 dB HL. There is a very useful chart based on Gelfand et al. (1990) that shows cut-off values for the acoustic reflex compared to true hearing threshold level.
19. One more thing – you mentioned wideband acoustic reflexes. What are they, and are they more sensitive than regular pure tone reflexes?
This is a modification of the technology used for wideband absorbance, in which the acoustic reflex is monitored across a broad frequency range using absorbance rather than admittance. The stimulus can be a click, which is then analyzed for different frequency regions, and the probe is also wideband. This technique produces better (lower) reflex thresholds, it can show the most sensitive region of the reflex in terms of frequency, and includes advanced signal averaging to reduce artifacts and noise. It isn’t yet available in those commercial instruments, but I hope it will be soon.
20. You’ve certainly provided me a lot of reasons why the immittance battery is a good thing, but I know some audiologists who don’t routinely do immittance tests. What’s your advice on that?
It is absolutely best practice to always consider doing immittance tests, and to decide based on the patient’s needs, while balancing cost-effectiveness. Have you ever been to a primary care physician who didn’t weigh you, do a blood pressure reading and listen to your heart, at a minimum, no matter what your complaint was? Oh and by the way, the weight and blood pressure was probably done by a medical assistant, right? Have you ever been to an optometrist who didn’t do a glaucoma screen even if you’ve had a gazillion normal ones before? So, while it is best practice to provide a standardized and thorough examination of our patients, we can use assistants to do parts of the exam, and we can decide when tests are unnecessary. If I have an established patient with previously normal middle ear tests who is in for a yearly hearing evaluation, I would do otoscopy and tympanometry because treatable middle ear problems are common, certainly more common than glaucoma. I would add reflexes if there was a change in hearing, or a new complaint like tinnitus. If they are in for hearing aid adjustment, I wouldn’t, unless they had a complaint suggesting middle ear or other problems such as tinnitus or dizziness. Determining when it’s appropriate is the difference between an audiologist and a technician.
Recommended reading:
Hunter, L.L. and Shahnaz, N. Handbook of Acoustic Immittance. (2013). Plural Publishing. *Normative tables referred to in this text are indicated.
References
Emanuel, D. C., Henson, O. E. C., & Knapp, R. (2012). Survey of audiological immittance practices. American Journal of Audiology, 21, 60-75.
Gelfand, S.A., & Piper, N. (1984). Acoustic reflex thresholds: variability and distribution effects. Ear and Hearing, 5, 228-34.
Gelfand, S.A., Schwander T., & Silman S. (1990). Acoustic reflex thresholds in normal and cochlear-impaired ears: effects of no-response rates on 90th percentiles in a large sample. Journal of Speech and Hearing Disorders, 55, 198-205.
Green, K. W., & Margolis, R. H. (1984). The ipsilateral acoustic reflex. In S. Silman (Ed.), The acoustic reflex: Basic principles and clinical applications (275-299). Ontario: Academic Press, Inc.
Hunter, L.L., Ries, D. T., Schlauch, R. S., Levine, S. C., & Ward W. D. (1999). Safety and clinical performance of acoustic reflex tests. Ear and Hearing, 20, 506–514.
Hunter, L.L., & Shahnaz, N. (2013). Handbook of acoustic immittance. San Diego: Plural Publishing.
Jerger, J. (1970). Clinical experience with impedance audiometry. Archives of Otolaryngology, 92, 311–324.
Kei, J., Allison-Levick, J., Dockray, J., Harrys, R., Kirkegard, C., Wong, J.,...Tudehope, D. (2003). High-frequency (1000 Hz) tympanometry in normal neonates. Journal of the American Academy of Audiology, 14, 20–28.
Lidén, G. (1969). The scope and application of current audiometric tests. Journal of Laryngology Otology, 83, 507-20.
Margolis, R.H., Bass-Ringdahl, S., Hanks, W.D., Holte, L., & Zapala, D.A. (2003). Tympanometry in newborn infants--1 kHz norms. Journal of the American Academy of Audiology, 14, 383-392.
McGrath, A. P., & Michaelides, E. M. (2011). Use of middle ear immittance testing in the evaluation of patulous Eustachian tube. Journal of the American Academy of Audiology, 22, 201–207.
Metz, O. (1946). The acoustic impedance measured on normal and pathological ears. Acta Oto-Laryngologica, 63, 1–254.
Straetemans, M., van Heerbeek, N., Schilder, A. G., Feuth, T., Rijkers, G. T., & Zielhuis, G. A. (2005). Eustachian tube function before recurrence of otitis media with effusion. Archives of Otolaryngology, Head and Neck Surgery, 131, 118–123.
Terkildsen, K., & Scott-Nielsen, S. (1960). An electroacoustic impedance measuring bridge for clinical use. Archives of Otolaryngology, 72, 339–346.
Cite this content as:
Hunter, L. (2013, September). 20Q: Acoustic immittance - what still works & what's new. AudiologyOnline, Article 12131. Retrieved from: https://www.audiologyonline.com