Editor’s Note: This text course is an edited transcript of a live seminar. Download supplemental course materials.
Introduction
Let's talk about educational audiology and what things we see in the classroom. This has become an area that has become more interesting to me lately as I am doing consulting and not working full-time in a clinic. I am spending more time in classrooms now than I did in the past, and I feel like I am learning a great deal. That is what I want to talk about.
Things are really changing in terms of what students need. Years ago when I first began, and maybe only 15 years ago, many children with hearing loss were identified late and began school with significant language delays. They required special schools or special classes. There were schools for the deaf. There were separate classrooms in mainstream schools for children with hearing loss because they could not manage in a mainstream classroom. That world has changed. Children are identified at birth. They get fit with technology within the first few months of life, and most of them are entering school with near-normal language levels. That is a wonderful thing, especially because 83% of children with hearing loss are being educated in mainstream classes. Today's children with hearing loss are more likely to achieve good educational performance than ever before, and that is very exciting for everybody.
As children get older, many of them start to decrease in their performance. As the language becomes more comples and as there become more critical needs for hearing, we see very significant decreases in children's performance. It is our job, as all the people who work with these children with hearing loss, to pay attention to what is going on and try to figure out what we have to do to improve performance.
Access
A number of different things affect what goes on in the classroom. How fast is the classroom instruction? Is the teacher going very quickly, or is there a lot of time for children to think about what is going on and to learn from each other? How rigorous is the curriculum? We know that, in some classrooms, the curriculum will be more rigorous than others, and if we have a hearing-impaired child who is in a classroom that has very high standards, that child has to be able to function differently than a child who is in a classroom where the expectations are low. How much are the children we are talking about able to glean from incidental learning? How much do they have to be told directly in order to learn, and how much can they learn from the people around them from overhearing conversations? What is their language like and how good is it? Can they hear the teacher well? Equally as important, can they hear other students? When other students comment on something the teacher has asked, can they get the message? Do they have the language foundation and vocabulary to understand everything that is happening in the classroom, or are they functioning at a significantly lower language level, therefore, not able to pick up what is going on in the classroom?
Is the technology the children are using working? Research from 1966 through 2011 is showing that more than 50% of the time technology in the classroom is not working the way we expect it to work. The sad part is that the statistics have not changed. The most common problem continues to be dead batteries, but unless we have someone in the school that can check the equipment daily, we do not know that a child's equipment is actually working.
Figure 1 shows a form that Karen Anderson (2013) developed, which I think is very helpful in thinking about how much a child is going to understand. If a child has an aided audiogram that is at about the 25 dB level, they have 40% audibility for soft speech in the classroom. For the teacher's voice , if they have a 25 dB aided audiogram, their audibility in the classroom is going to be 81% to 98%. But if they are hearing at 35 dB, they only have 10% audibility for soft speech and 45% to 60% audibility for the teacher's voice. Think about how much that means they are missing. If they have 25% audibility for soft speech, that means they are not able to hear the children around them, and they are not going to have good incidental learning.
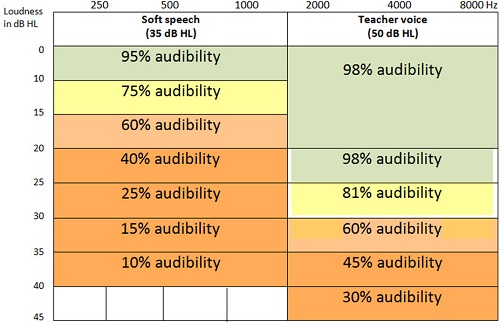
Figure 1. Comparison of audibility as a function of hearing threshold in dB HL (Anderson, 2013).
Figure 2 is an audiogram which gives you a sense about where this child may be hearing. At first glance, this child seems to have a pretty good audiogram, yet they are still not getting everything that they need to get.
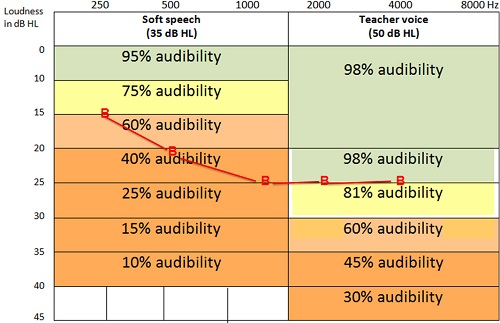
Figure 2. Audiogram overlaid on audibility chart; even a slight-to-mild audiogram limits audibility (Anderson, 2013)
Classroom acoustics are critical. If you were in a classroom with one 40-watt light bulb, you know you would not have adequate lighting. What about the acoustics of that classroom? We know that acoustic treatment in a classroom is critical. We also know that it only costs between 1% and 5% of the construction budget, but meanwhile only 10% to 30% of classrooms meet the current ANSI (American National Standards Institute) standards for noise. Thirty percent of the classrooms are judged to be too noisy by educators, primarily the result of heating, ventilation, and air conditioning systems. We also know how critical noise is. Children under 13 years of age are the children most challenged by noise. Those are the critical years for beginning academic learning. If a child does not get what they need to get in those first six to seven years of school, that child is not going to be able to compete when they get to high school. We need to always pay attention to how much noise there is the classroom. We know that teachers have to talk loud in order to overcome the amount of noise in the classroom and they have significant problems with noise in their voices. Teachers have a 20% greater risk of damaging their voice than in other professions.
When a teacher raises her voice to be heard over the noise, what sounds are heard? Vowels. Vowels are louder. Those are the sounds these hearing-impaired children can hear pretty well by themselves, but the consonants do not get louder. You cannot make /s/, /f/, and /t/ louder by shouting. We know that strategic seating is critical. In order to hear the teacher's voice, the teacher’s voice has to be 15 dB louder than the noise around them. That means that the child has to be really close to the teacher or has to have a really good, working FM system. We know that in children who are normal hearing and are not native English speakers, the effect on them for listening in the classroom is the equivalent effect of a 25 to 40 dB hearing loss. What does that mean for a child with a hearing loss? It is a significant difference.
Effect of Acoustics on Classroom Learning
Classroom acoustics affect learning in a lot of ways, such as how fast and how well a child learns. The rate at which a child learns is going to be a significant factor. How persistent the child is and how well the child can pay attention and pull themselves together in a noisy classroom will make an enormous difference. There have been a number of research studies which have shown that children who are in classrooms close to noisy areas like subways in New York or freeways in other places have a one-year drop in academic equivalent for every 10 dB of traffic noise in the classroom. We need to pay attention to classroom acoustics and see whether we can improve them.
Children do not habituate to noise. In fact, they tend to tune out. If you cannot hear, you cannot hear; that is the long and short of it. One of the things we want to know is what we can do to fix that and how many children should have FM systems. We need a good high-quality FM system to work. Jace Wolfe did a study comparing the Phonak Dynamic FM with audio enhancement to personal FM only. He discussed this study at the Phonak pediatric conference in 2012 (Wolfe & Vickers, 2012), and the results should be published soon. With personal FM and Phonak dynamic FM, the children did best. We absolutely know that if a child is hearing only with a soundfield system, no matter how good the soundfield system is, they are not getting enough information. Children with hearing loss absolutely have to have personal FM systems in order to hear well in the classroom. The gold standard for how well a child should hear means that at any child with hearing loss has to at least have a personal FM system, and ideally a wearable personal FM system, with a soundfield FM system.
Here are some data from Erin Schafer and Mary Pat Kleineck (2009) looking at the benefit of FM with a cochlear implant versus cochlear implant alone (Figure 3). It is interesting to me to see that they have compared a personal direct audio input FM with the desktop FM with the soundfield FM. They are clearly showing that a personal FM results in significantly better speech perception than a desktop or a soundfield system. The soundfield system has the same problem of distance from the microphone.. The speaker is just in a different place. The desktop system, even though it is sitting right in front of the child, is still not providing the appropriate speech perception. If the question is, “What kind of FM does a child need in the classroom?” the answer is always direct audio input.
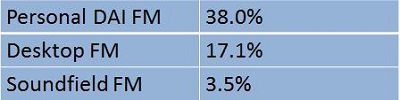
Figure 3. Benefit in terms of increase of speech perception scores using FM systems over CI alone (Schafer & Kleineck, 2009).
What is Required for Success
Let's talk for a minute about what is required for success. Every child must be evaluated to know how they are doing. We cannot assume. For a child who comes into school with delays, the goal is obviously to close those delays. If a child comes in with typical skills, the goal is to keep those skills where they are so that the child can stay on par with their peers. The Individuals with Disabilities Education Act (IDEA), as we all know, specifies that we need to support the development and use of technology, including assistive technology devices for maximizing accessibility for children with disabilities. For children who have hearing loss, this also includes providing a communication system where the child can hear, and if the family has chosen listening and spoken language, FM access is part of the communication system that these children will need. Equal access is the goal of IDEA, and that is our goal in allowing our children to function well in the classroom. Our goal is to give them equal access so that they can hear what they need to hear to learn.
For the children to succeed and learn what they need to learn in the classroom, they need to be able to understand the teacher. They need to be able to express their thoughts and ideas. They need to be able to tell us what they are thinking. They need to know when they do not understand, and they need to ask for help if they do not understand. They need to have social relationships with their classmates. If they do not, then school is not going to be successful.
What does the school staff need to know in order to make this work? The school staff needs to understand what is involved in helping children succeed. They need to know what is involved in listening and in developing conversational skills. They need to develop a hierarchy of skills the child needs to develop, and that the teacher needs to recognize when a child does not understand and help the child determine what to do when they do not understand. The school needs to understand what they can do to help build skills in different listening environments and in different academic settings. They need to help this child develop self-advocacy skills so that the child can learn and move on.
Classroom Evaluation
What kinds of skills does a child need to develop for communication repair strategies? First, they need to be willing to persist when they do not understand. They cannot quit. They need to have the ability to try to continue to communicate. Second, they need to recognize that there has been a communication breakdown, and then they need to do something about it. If they do not know that they have not understood, then they cannot even begin to try fixing it. They need to develop some communication options, ways to say “I did not hear that. Can you say it again?” or “I am sorry, I did not understand. Can you say it in a different way?” We need to give children practice in doing that and help them understand it. Anderson and Arnoldi (2011), in their new book on school issues, have some really good information. The SCRIPT program (Student Communication Repair Inventory Practical Training), which is in their book, is something that you might want to look at for helping children develop communication repair strategies.
It is important that we know how a child is hearing. How does this particular child's hearing loss impact how they participate in the classroom? What are they hearing? Does a child have sufficient acoustic access to be able to hear what is happening (Figure 1)? How well do they hear with the technology? What are their aided thresholds, and are they hearing well throughout the frequency range or only in the low to mid frequencies? What has been happening in the classroom to accommodate the child's acoustic access? Are they making an effort to keep the classroom quiet? Is there a rule that you do not sharpen pencils while someone is talking? How is the student’s academic achievement compared to their peers? It is not all right to say he is doing well for a “deaf child,” because that is not our goal here. Our goal is to have this child doing as well as all of the children around them. Is this child continuing to make progress? How are they compared to their peers? Is this child consistently at the bottom of the class? Is this child being sent on to the next grade even though they do not have the skills to really compete equally? What kind of interventions does this child need in order to make them do better in the classroom? We need to know that, and we can see part of that when we observe. Part of it we get by looking at the academic records.
What about their communication skills? How well does the child understand what is happening in the classroom? What is the child’s language level and how does it compare to the other children in the classroom? It is not enough to say this is how this child’s language compares to nationwide surveys of where a child’s language should be. This child is in a particular classroom with particular children and has to compete with those children. It is not how well this child compares to everybody in the United States. It is how this child compares to the children who are sitting next to him, so that he can learn to function with those children. Is his language as good as those children? Are the classroom's expectations the same for this child as they are for other children?
What are the child’s functional skills? How does the student advocate for himself, and what does the child do if he needs some compensatory help, when he is not getting what he needs to get? Does he look over at his neighbor to see what page they are on? Does he get answers from somebody else, or is he trying to do the work himself? How does he respond to breakdowns in the classroom? When he does not know what is happening, does he get upset, or does he continue to proceed and try to figure out a way to solve the problem? Is this child using an interpreter, and if he is, how is that working out? Is he getting the academic material, but not getting socialization skills because his language is not good enough and because the interpreter is the primary communicator? All of those things need to look be looked at. If the child has an interpreter and is having trouble communicating, what can we do to improve that situation?
What about the child's social and emotional skills? It is not easy to be a child who is different than the other children in your classroom. How is this child handling it? What is the school doing to compare the hearing impaired child to peers, and to use that information to develop a management program? How is it helping? What can we do to improve children’s social skills so that they understand and communicate better? Social skills have a large language component. Does this child have the language to socialize well? There are informal assessments and formal assessments that we can do. We obviously can review the student’s records to see what is going on in the classroom scores. We can observe in the classroom to see how the child is learning. How is the child attending? How is the child socializing? We can check with the child to see whether they understood what was being said just recently. We can talk to the parents, teachers and the hearing-impaired children and ask them how they are doing. We can also talk to their friends in the classroom and see what their friends think. We can look at homework and spelling tests and all the academic work in the classroom and see how what they are doing compared to other children.
One critical thing we want to know is if the child is following what the teacher says. When you sit at the back of the classroom, you can see whether the child is looking at the teacher, looking at the paper, or whether their mind is wandering. If their mind is wandering, it is likely because they are not hearing. We need to know that, because we need to know what we have to fix. Can this child follow directions without assistance or does he need his neighbor’s help? When the teacher says go to page 43, does the hearing-impaired child have to look at their neighbor and see what page that child is on? Does this child have to check to see what is happening around him? Does the child answer questions appropriately, or is the question that the child answers not really the question that was asked? Does he volunteer or does he just sit back? Some of that is personality, but a lot of it is confidence in your ability to communicate. Does the child listen to what other children are saying or when other children are speaking, or does the child wander off because they know they cannot hear them? Where is the child seated? Are they seated in a place where they can both hear and see what is happening? How does the child manage as the day progresses? Does the child become more and more tired and just have a very hard time tuning in? Is the child socializing?
What about the teacher? Is the teacher using an FM microphone? Is she using it appropriately? I have done two classroom visits recently, one in which the FM microphone was sitting on the teacher’s desk, and she was not sitting at her desk, and in the other the FM microphone was at the teacher’s waist. How much is that child going to hear? Not enough. Does she know to turn it on and turn it off when she is talking to other children and it is not the hearing-impaired child's business? It is annoying to have to listen to somebody talking about something not related to you. Is there a pass mic? Is the pass mic being used appropriately? Are the children waiting for the pass mic in order to speak? Is it a quiet room or is it a noisy room? What about street traffic? What about the pencil sharpener? What about the air-conditioning? All of those things matter.
Does this child manage with a standard test time or the does the child need extended test time? How well is the child able to keep up during the time that the child is listening to whatever is going on in the classroom? Where does the student stand academically in this particular classroom? Is this child in the middle, which is what we would hope? It would be lovely to be at the top, but we want to know where this child stands and what the teacher's goals are for this child. Does the teacher want this child to learn at the level where the child is, or does this teacher say or think that that child is hearing-impaired and thinks about what we can expect? We really want to know what the teacher thinks about how the child is functioning and what kind of accommodations is the teacher willing to make for this hearing-impaired student. Will she repeat or does she get annoyed?
I did a classroom visit for child with a cochlear implant not long ago in which the teacher was so clearly annoyed, even with an observer in the room, about the need to repeat. When the child raised his hand and said, “I am sorry, I do not understand.” She said, “I will talk to you afterwards.” That is an unfortunate situation for anyone who is trying to learn.
It is important to know who is conducting the observation and what that person is looking at. We want the person who conducts the observation to be able to look at classroom acoustics, at what the child is hearing, at how the child's language compares to the language level in the classroom, what the child’s socialization skills are, and how the child is communicating with peers. The person has to have a breadth of knowledge, but the observer also has to understand the acoustics. If it is an auditory-verbal therapist, a teacher of the deaf, or an audiologist, we know that they are going to have that information. If it is the special education supervisor, they may not have information about audition or recognize what is going on and where the FM should or should not be. Those are all things we have to think about when we are looking at a classroom observation.
When we have completed the classroom observation, what are we going to do next? Do we need to educate the teacher about how to use the FM, and when to turn it on and off? If there is not a pass mic, we can counsel about repeating the comments of the children in the classroom, and how to know when a student is missing something and what to do about it. When you do a school visit, we also need to observe speech-language services. While some speech-language pathologists have a lot of information about hearing loss, the majority of speech-language pathologists have very little experience with hearing loss. Many have not been exposed to children with hearing loss. If they took a class in graduate school, it was probably only part of a class that worked on teaching children to use audition. We need to know whether they know how to help children with hearing loss develop auditory skills. Are they helping to build the children’s auditory skills so they can learn new things and what are they focusing on? Are they working on language using an auditory model? We hope they are working on language, but they need to be working on audition also.
Any child with a hearing loss will benefit from the services of a teacher of the deaf. The teacher of the deaf has lots of responsibilities. Certainly, the teacher of the deaf is there to observe what is going on the classroom, see how well the child understands, and help the classroom teacher use the FM appropriately, but once a child gets into second or third grade, a significant part of what a teacher of the deaf should do is a preview and review of academic material. A lot of the time that is not happening. We want to know that the child is getting the information that they need. We want to know that they are hearing the things they need to hear and that they have the language. The reason for preview and review is to make sure that the child has the language ahead of time so that they can learn from the material presented by the teacher in the classroom. That is a critical part of the role of the teacher of the deaf. Even if there is not a full-time teacher of the deaf, the boards of cooperative educational services (BOCES) in the area should be able to provide a teacher of the deaf to come in and provide preview and review services on a regular basis.
We need to inform special education staff about the observations and make sure they understand what the good and bad things are that happened here and figure out what we have to do to make sure that this child gets what they need in the classroom. In fact, it is the special educators who are going to be the people who have to carry out the program in the end.
Let's talk for a minute about how we know when hearing loss may compromise a student's performance in the classroom. Something very obvious would be if they give the wrong answers to questions. You know they are not hearing. If they have to ask for repetition a lot, you know they are not hearing. If their attention wanders, they do not have good social skills with their peers, or they get very tired as the day goes on, those are all suggestions that this child is not hearing well in the classroom. Their hearing loss is compromising their ability to manage.
Case Study: Matthew
Let's talk about Matthew, who is nine years old with severe hearing loss and uses bilateral cochlear implants. He is mainstreamed and in third grade. His cochlear implant center did an evaluation, and they reported that he was doing beautifully. He got 98% speech perception using the PBK lists with the right CI, the left CI, and binaurally. The mom came to me for consultation because she felt he was really struggling. He has these scores that look like he is doing terrifically (Figure 4). The first thing I do is I look at this and I say, “Well, they are using the PBKs, which is a kindergarten word list. With a kindergarten vocabulary, this child in the third grade is doing very well.” I do not actually care how he does with the kindergarten vocabulary, because that is not going to help us know what he is really hearing in the 3rd grade classroom.
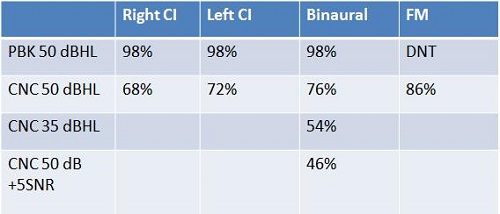
Figure 4. Matthew’s speech perception scores for the right CI alone, left CI alone, binaural and FM conditions.
Even worse, when the school got this report, the school said he got 98% performance in all test conditions, (which was actually only testing at normal conversation in quiet), so his hearing loss is cured and determined that he no longer needed services. Now what are we going to do? The first thing we did was retest him. If you look at Figure 4, you can see that he did very well at normal conversation (50 dB HL) using a kindergarten word list. But when we used the appropriate word list at normal conversation for a child in third grade, we are seeing that his performance is significantly poorer; 68% for the right CI, 72% for the left CI, 76% for the binaural condition, and 86% with the FM system. Still not terrific. At soft speech (35 dB HL) he only has 54%, and in noise he has 46%. We know right away this child is going to be having a hard time in the classroom.
He had a speech and language evaluation. If you look at the standard scores (Figure 5), it looks like he is doing okay, but then when you start looking at the percentile rank and the age equivalent, you can see at least four areas where he is performing significantly poorer than we would like him to perform: pragmatic language, sentence completion, grammatical judgment, and inference. What does that mean about how he is going to be managing in a classroom? If his pragmatic language, his sentence completion, and his grammatical judgments are poor, that means there is something very wrong, and this child is not going to be functioning the way we want him to function.
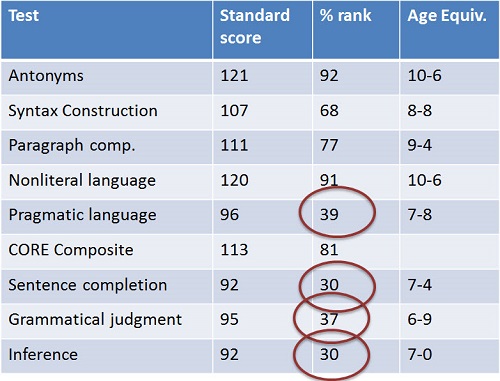
Figure 5. Speech-language evaluation scores.
Then we had a psycoeducational evaluation performed (Figure 6). If you look at just the standard scores, everything looks pretty good. He is in the 90th to 100th percentile. But look at the percentile ranks, and you will see that there are significant deteriorations. There are places where he is not hearing well, and this is a significant problem.
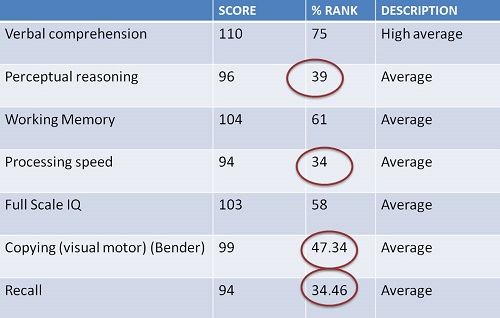
Figure 6. Scores for Matthew’s psychoeducational evaluation.
Here is another situation. We look at Matthew's scores when he was five, and then again repeated when he was nine. We can see a very significant deterioration in certain areas (Figure 7). What does this mean about how Matthew is managing in a classroom? Is he is doing okay? He may be doing okay, but we have to start worrying now when we look at his scores over time and see that in several areas, his skills are deteriorating.
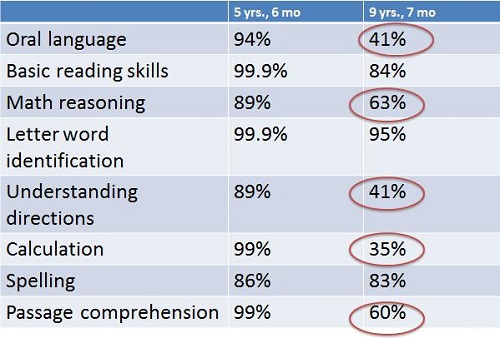
Figure 7. Comparison of scores at 5 years 6 months and 9 years 7 months.
Who is monitoring his performance? Is there someone at school who is paying attention to how Matthew is doing, looking at his progress over time and seeing what is happening? Whose responsibility is this? Is it the special education office? Is it the teacher of the deaf? Is it the speech pathologist? Is it the educational audiologist? Someone has to be responsible. What ends up happening, for the most part, is that people are looking at where Matthew is at that moment and not looking at the big picture. As a result, we have a child who is not doing as well as he should be doing. It ends up being the parents’ responsibility. It ends up being the parents who have to say, “Something is wrong here. What do we need to do about it?” Not all parents are capable of doing that.
What is the role of the clinical audiologist? What do we have to do if we are seeing these children outside of the school system? What is our responsibility for making sure that a child is progressing? Are we only responsible for fitting hearing aids and saying someone else has to worry about this? Unfortunately that is not a good way to progress. Everyone who is working with a child needs to put together the pieces and figure out how a child is progressing and what to do next.
What are we going to recommend for Matthew? Obviously he needs an appropriate audiological evaluation, which means doing speech perception testing using age-appropriate speech-perception tests. We need to make sure that he is using the FM in all his classes and that he is using a pass mic. We need to make sure that a teacher of the deaf is there to preview and review, and in Matthew’s case, the teacher of the deaf visited the classroom, but was doing no preview and review. That was being left to his mother. We need to see what we can do about modifying the classroom acoustics, and if Matthew needs extended time for tests, we need to see that it gets added to the IEP. There are some specific speech and language and listening goals identifying areas of weakness that have to be listed and worked on. The areas that that Matthew demonstrated weakness in speech and language and in the psychoeducational evaluation are the areas where Matthew needs specific work. Some of them will be the responsibility of the speech-language pathologist and some of the responsibilities will be those of the teacher of the deaf or the classroom teacher.
One of the things that sometimes happens, and Matthew is probably a good example of this, is that if you look at his standard scores, it looks like maybe he is not entitled to services. But I think it is important to review the specific tests to look at areas of weakness and to develop a plan to remediate those areas of weakness. In my experience, we can usually convince the school to do what needs to be done if we can show them the specific areas of weakness.
How do we decide who gets intervention? If a child is more than 2 years delayed, then we know that the child is entitled to all kinds of accommodations and individual instruction by a teacher of the deaf. If a child is 1 to 2 years behind in grade level, then they may get some special instruction services, and the teacher of the deaf may function in a push-in model. If a child is performing at or above grade level, the child is almost punished for that activity, because they will not get assistance unless we start to see the child failing. That is something that we would all like to avoid. If everyone who is working with the child monitors the child’s performance and picks up on areas of weakness before they start to deteriorate, then we are in a much better place to be able to get the school to do what we think the school needs to do to prevent the child from starting to fall behind.
Figure 8 is a list of checklists that are available, all of which are very useful in keeping track of what a child hears and how a child is performing in a variety of situations. By using the checklist over time, we can see whether the child is continuing to progress or if the child starts to deteriorate.
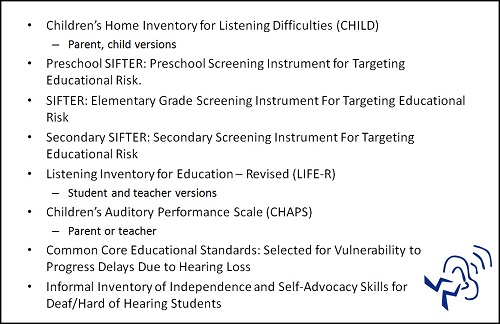
Figure 8. Educational checklists and questionnaires to monitor listening progress and risk.
Teenagers
Teenagers are a whole special category. One thing that is helpful is to talk to teenagers about the lifelong impact of hearing loss. When children reach the point where they start removing their hearing aids, we know they are doing it for social reasons, and it is a big issue. It may be helpful to tell children that adults with hearing loss who wear hearing aids earn 50% more during their lifetime than those who do not wear hearing aids and try to get by. Some recent research has indicated that 30% of people in prison have hearing loss, meaning that people who do not hear sometimes choose to do things that might not be in their best interest. They are making some bad choices. We let children know that it is not just about how they look, but there are implications for not hearing what is happening, and it is an issue. Let’s talk about a couple of children and what we might do to help them figure this out.
Say we have a 10-year-old child who comes to school and says he has left his hearing aids at home. When he goes home, he tells his parents he left his hearing aids at school. How do we deal with this? “Why is this child doing this?” is the first question. What do we need to do to change his behavior? We can talk to this child. We need to discuss this with him. Start with, “You must really be upset about wearing hearing aids. It must be difficult in school.” One of the things that we have to do is say to children that we know this is hard, that it stinks, and it is not fair. We have to give them the information that they need so that they understand that we are not saying they have no right to be upset about it. They are entitled to be upset. “It really stinks, but what can we do to make it easier for you?”
What do we need to do to make sure that children do well in school? First we need to make sure that the technology is providing enough assistance. That means that with the technology, we need aided thresholds at 20 to 25 dB, throughout the frequency range, whether that is with hearing aids or cochlear implants. We need to make sure that the technology is being used appropriately. Is the teacher using the FM? Is she turning it off when she is talking to other children? Is there a pass mic that is being used appropriately? If there is not a pass mic , does the teacher understand that she has to repeat back everything that is said? We need to educate the school staff about what effects hearing loss have on a child, specifically what it means for language and academic learning. They need to understand that as a child starts to deteriorate in performance, it is a factor that is going to affect him for the rest of his life. They need to understand that language is cumulative, and if a child is not getting cumulative language skills, their performance is going to deteriorate. They need to know what the child’s skill level is and figure out what they have to do to improve performance.
When we are testing to know if the technology is working, we need to be testing normal conversation, soft conversation, and speech in noise. Someone asked me what level I recommend for testing speech in noise, both with the technology alone and with the FM. I test at +5 signal-to-noise ratio using four-talker babble, because that is most typical of what is happening in a classroom. We need to make sure that there is preview and review of academic materials by a teacher of the deaf or a special education teacher, to make sure the child has the academic language so they can learn in the classroom. We need to be sure that the child recognizes when they do not understand so that they can ask for help. We need to monitor their social skills, because if you do not have friends, you are not going to be a happy person.
We also need to arrange for support groups. The one problem with hearing-impaired children being in mainstream settings is that they frequently do not have the opportunity to know other children with hearing loss. They do not really have peers. As clinicians who are working with children with hearing loss, we need to arrange an opportunity for them a few times a year to meet with other children with hearing loss to share experiences. Just knowing that there are other children out there who have the same situation, the same frustrations, who are misunderstanding what is going on in the classroom, is very empowering for children. Running support groups for children with hearing loss is one of the most fun things that I do and love. It is something that I would encourage you to try and do if at all possible.
Here are some references for some of the things that I talked about today. The Anderson and Arnoldi (2011) book is great for anyone working in a classroom. It is really something that I think you will enjoy if you work in a classroom setting. It is a big fat book with a lot of information. You can easily find it, and it is wonderful. It will be useful to you. Another resource you may consider is Carol Flexer’s and my Pediatric Audiology book (2008) and our Casebook (2011), both published by Thieme.
Questions and Answers
Would you test an FM in noise as well as in quiet?
The answer is absolutely yes. Yes, you should be testing the FM in noise.
What do you recommend for signal-to-noise ratio when testing with the FM?
I strongly recommend that you test normal conversation, which is 50 dB HL, soft conversation which is 35 dB HL, and at least normal conversation of 50 dB at a +5 dB signal-to-noise ratio. Here is my reasoning. First, you want to be sure that the child is hearing normal conversation, which means they will hear a person who is three to four feet in front of them. You also want to know that they can hear soft conversation. Soft conversation means they can overhear and hear things from a distance. Eighty percent of what a child learns is learned by incidental hearing, by overhearing conversations around them. If they cannot hear at 35 dB, they are going to miss that. If a child has to learn everything by direct teaching, they are going to be missing a great deal.
Speech in noise is significant because, in fact, the world is very noisy. I use four-talker babble because it is most typical of what a child is listening in. We are not listening to speech noise in the background. Speech noise from the audiometer is easy to tune out. Four-talker babble is not easy to tune out. We really need to be able to see how a child is hearing in those very difficult situations. If a child has good hearing, I would also try to get information about how the child is hearing for soft speech in noise, because that is also going to provide significant information. I think the information that we get for how a child hears soft speech and speech in noise is more important than how a child hears normal conversation, because it is going to tell us how much they can expand what they are hearing.
What assessments were used to test Matthew?
The tests from the 5-year-old and 9-year-old were the same tests. It was the Woodcock-Johnson, and there were some speech and language evaluations also. There are a variety of different tests that were used that are useful in looking at these children over time.
A lot of the checklists are available through the Education Audiology Association’s Web site, and others are available through Karen Anderson’s Web site. Almost all of the checklists are easily available and are available free. There is no reason not to be using them.
Why do you use 50 dB instead of 65 dB for speech testing?
Well, 65 dB is loud speech. I actually do not care how a child hears loud speech, because they do not have enough exposure to it in the classroom or at home. They are not hearing loud speech when they are trying to learn. Normal conversation is 50 dB HL. You also have to test soft speech at 35 dB HL. You can test loud speech, but it is not going to tell you how a child is learning, because if a child is relying on loud speech, they are not going to be able to manage in that classroom. There is just not enough consistent sound occurring at that level.
Many times educational audiologists have time constraints. What would your order of testing be on a have-to basis?
That is a very good question. I am going to say something that is going to be really out there. I am assuming that there is a clinical audiologist who is monitoring how a child is hearing, so unless the educational audiologist is the primary audiologist, I do not think you need to worry about the child’s unaided thresholds. You need to know how the child is hearing in the classroom. You need to know what the child's speech perception is at normal conversation, soft conversation and speech in noise, so you can tell the people in the classroom what to expect. If the clinical audiologist has done that unaided testing, and we hope that he or she has, then you have the information and you can go in and monitor the equipment. Your primary responsibility is to know how the child is hearing and to make sure the equipment is working every day. I know you have time constraints, but that is what I would say are the most important things.
What does signal-to-noise mean?
Signal-to-noise: If it is +5, it means the signal is 5 dB louder than the noise. I would have the speech at 50 dB and the noise at 45 dB. If you have a signal-to-noise ratio of 0, it means speech and noise are at the same levels, so they would both be at 50 dB. Normally, we test with speech being a little bit louder than the noise, because a +5 signal-to-noise ratio is what is typical in a classroom setting.
Do you have good speech test results for soft speech with cochlear implants versus hearing aids?
It does not matter what their technology is, it matters how they hear with it. A child with a moderate hearing loss should be hearing at 20 to 25 dB across the board. A child with a cochlear implant who has a severe to profound hearing loss should be hearing at 20 to 25 dB across the board. However a child is hearing with their technology, I want them to hear with their technology as well as they can hear. It does not matter whether it is a hearing aid or a cochlear implant. If you have a child who has a profound hearing loss who is wearing a hearing aid and does not have a cochlear implant, that child is not going to hear soft speech. That is a different problem. That means it is time to change technology. That child is going to be very dependent on an FM, probably full-time.
Can you explain what a pass mic is?
A pass mic is the second microphone in the classroom which is a handheld pass-around mic. You pass it from person to person for people who are talking. So whoever is speaking waits for the microphone and then talks into it, so the child with the hearing loss is hearing that person's voice the same way they are hearing the teacher's voice. The advantage of a pass mic is critical. I think that it is important that everyone understands that it is not a casual thing. It is a big imposition on the teacher to have to repeat everything that is said in the classroom, but if we do not do that, then the child is not going to hear. It is important to be sure that we do that. If you do not have a pass mic, see if there is anything you can do about obtaining one.
Is there an update on the survey about bullying in children with hearing loss?
The answer to that is yes, and we are doing a workshop at AAA in April about that. We will have more information at that time. It will be published after that.
What is a push-in model?
A push-in model means that the teacher of the deaf goes into the classroom to do the teaching, rather than a pull-out model in which the child come out of the classroom for services. Those models are valuable at different times. If you are trying to help a child learn to make better use of the classroom, then a push-in model is a good thing, because the teacher can see where the child is struggling and help everybody understand what to do then. When a child needs more help, a pullout model is where we need to go.
References
Anderson, K. (2013). Speech audibility audiogram for classroom listening. Retrieved from https://successforkidswithhearingloss.com/impact-on-listening-and-learning/speech-perception
Anderson, K. & Arnoldi, K. (2011). Building skills for success in the fast-paced classroom. Hillsboro, OR: Butte Publications, Inc.
Madell, J. R., & Flexer, C. (2008). Pediatric audiology: diagnosis, technology, and management. New York, NY: Thieme Medical Publishers, Inc.
Madell, J. R., & Flexer, C. (2011). Pediatric audiology casebook. New York, NY: Thieme Medical Publishers, Inc.
Schafer, E. C., & Kleineck, M. P. (2009). Improvements in speech-recognition performance using cochlear implants and three types of FM systems: A meta-analytic approach. Journal of Educational Audiology, 15, 4–14.
Wolfe, J., & Vickers, D. (2012, December). New trends in soundfield. Presentation at Advances in Audiology - Tomorrow's Solutions for Today's Challenges sponsored by Phonak, Las Vegas, NV.
Cite this content as:
Madell, J. (2013, May). Educational audiology: From observation to recommendation. AudiologyOnline, Article #11853. Retrieved from https://www.audiologyonline.com/